I have completed 15 days of Dry January 2023. Dry January began in 2013 as a campaign sponsored by Alcohol Change UK to encourage people to abstain from alcohol for the month of January. Ten years later the number of participants has grown exponentially and people all over the world are supporting each other for 31 days of avoiding drinking and examining their relationship with alcohol.
I have completed 15 days of Dry January 2023. Dry January began in 2013 as a campaign sponsored by Alcohol Change UK to encourage people to abstain from alcohol for the month of January. Ten years later the number of participants has grown exponentially and people all over the world are supporting each other for 31 days of avoiding drinking and examining their relationship with alcohol.
Dry January is not really related to my diabetes but like with everything else in my life, diabetes always comes along for the ride.
There are many criteria for determining alcoholism or at least alcohol abuse. An online search for those terms will give you lots of info–maybe more than you want to know. I don’t think that many others look at me and see a problem drinker and I don’t drink enough to get visibly drunk. But I know that I have been drinking more than the weekly wine allowance for women (7 servings @ 5 oz) and it is a fallacy to pretend otherwise.
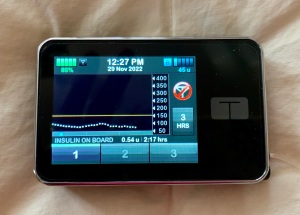
I can’t really say that I am currently experiencing many negative consequences from my nightly wine. But there is no doubt that alcohol increases my risk for liver disease, breast cancer, pancreatitis, and all sorts of bad things. I have gained unwanted weight in recent years with the empty calories of wine on top of a slowing senior metabolism. Diabetes-wise, I suspect that my problem with overnight high blood sugars is related to the interplay of alcohol and food. For sure I live with self recrimination.
My drinking history is unremarkable. I drank a little beer in college but not much. My husband and I rarely drank in the early years of our marriage and definitely not at home. When my youngest son played hockey in high school (circa 2000) we started going to bars after games with other parents. That must have been my introduction to wine because I don’t like beer very much. Hard liquor has never been part of my life and because of my Type 1 diabetes, I have rarely ordered anything with mixers.
So here I am in 2023 drinking too much wine. What happened?
 Things changed gradually and daily drinking wasn’t part of my life until 6-7 years ago. Boxed wine likely skewed my quantity control as the spigot of these boxes dispenses a seemingly never-ending supply of delight with no keeping count. I slowly incorporated a glass of wine into my late afternoon regimen. It was so obvious that when I poured a glass of wine at 5:00, the dog knew that it was time for her dinner. But 5:00 often became 4:00 and occasionally earlier. Ironically my blog became a trigger because it’s quite nice to sip wine while writing about diabetes and my journey into seniorhood. Boredom has also been a factor with alcohol being a nice change from a day filled with water and diet soda. The pandemic definitely magnified my boredom with a lot more time at home and sometimes not much to do. And I like the taste of wine.
Things changed gradually and daily drinking wasn’t part of my life until 6-7 years ago. Boxed wine likely skewed my quantity control as the spigot of these boxes dispenses a seemingly never-ending supply of delight with no keeping count. I slowly incorporated a glass of wine into my late afternoon regimen. It was so obvious that when I poured a glass of wine at 5:00, the dog knew that it was time for her dinner. But 5:00 often became 4:00 and occasionally earlier. Ironically my blog became a trigger because it’s quite nice to sip wine while writing about diabetes and my journey into seniorhood. Boredom has also been a factor with alcohol being a nice change from a day filled with water and diet soda. The pandemic definitely magnified my boredom with a lot more time at home and sometimes not much to do. And I like the taste of wine.
Where does diabetes fit into this?
I’ve had Type 1 (autoimmune, insulin-dependent) diabetes for over 46 years. I am relatively healthy with none of the dreaded nerve, eye, kidney, or cardiac complications. But diabetes is not easy and I spend a lot of time not eating things that I would like to eat. Yes, supposedly I can eat whatever I want, but it is a PITA to balance insulin with large quantities of bread, pasta, cereal, rice, sweets, and other higher carb foods. It rarely turns out well. I can drink white wine with at most a minor impact on my blood sugar. One could argue that a glass or two of wine in the late afternoon is better than a bunch of crackers. Ah, sounds like self-delusion.
The biggest physical effect of Dry January on my diabetes has been that my total daily dose of insulin has gone down dramatically. On most days my basal insulin has been reduced by over 25%. My overall blood glucose numbers are improved but I am unsure whether that is because of no wine or just eating less.
The biggest psychological effect of Dry January on my diabetes is that the discipline of alcohol abstinence is making it easier for me to be disciplined with my eating. Frankly I expected that it might go the other direction and that I would eat junk to replace wine One of my goals this month is to lose a couple of pounds and I hope that the combo of no wine and less food/fewer carbs will make that possible.
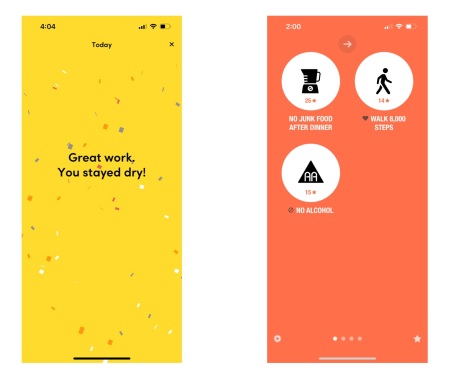
A month ago I purchased the Streaks app in anticipation of Dry January. There is nothing better than a phone icon patting you on the head for a job well done. My first task was eating no junk food after dinner. Apple slices and string cheese are okay, but no cookies, candy, or ice cream. That coupled with no alcohol has eliminated blood sugar spikes overnight. Fortunately I haven’t struggled much with reducing food or alcohol this month and that has been a surprise.
I probably sound like a goody two-shoes saying this is easy and that is easy. What Dry January and restricting junk food after dinner emphasize is that I am good at none and terrible at one. The potato chip commercial that says “Bet you can’t eat just one” is directed at me. I don’t stop at one cookie. I don’t stop at one piece of candy. I don’t stop at one glass of wine. But I can do none.
Why do Dry January? Why not just take a vacation from drinking? I do well with structured goals and get support from nitty-gritty scorekeeping. I go to the calendar in the Try Dry app every evening and after my report of no drinking, I get a bright confetti-laced congratulation. The Streaks app displays how many days I’ve succeeded with my goals. Silly but motivating rewards. Dry January gives me accountability. I said I would do it; therefore I will. For myself and for everyone else participating in the program.
Another positive with Dry January is that there is a predefined goal and an endpoint. The success of Dry January 2023 will not be determined by what I do on February 1. The challenge is to avoid alcohol from January 1-31 and I am confident that I can do that. But I am already concerned about February 1. Can I move from the structure of Dry January to continue not drinking in February? If I choose to return to wine, can I moderate my quantities? Things that were easy for 31 days will probably become difficult if they turn into forever tasks.
At the beginning of the month I did not have the goal of avoiding alcohol for longer than a month. Two weeks later I like not drinking. I feel good. I am sleeping better. My blood sugars are slightly better. I think I am losing weight. I have one less thing to feel guilty about.
On February 1, maybe I can keep this up for a while longer. I don’t know if I will want to or if I can. But if I do, it will be by avoiding one and staying with none. Not exactly moderation but a good start.
TBD….
*******
Resources:
Dry January Info: https://alcoholchange.org.uk/help-and-support/managing-your-drinking/dry-january
NIH Drinking Levels Defined: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking
National Institute of Alcohol Abuse and Alcoholism: https://www.niaaa.nih.gov/
Alcohol’s Effect on Health: https://www.niaaa.nih.gov/alcohols-effects-health/alcohols-effects-body
The Huberman Lab podcast What Alcohol Does to Your Body, Brain & Health: https://hubermanlab.com/what-alcohol-does-to-your-body-brain-health/
CDC Alcohol Fact Sheets: https://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm


 I was given the opportunity to read and review Stacey’s second book, Still The World’s Worst Diabetes Mom. In general I turn down most opportunities of free stuff because although I usually write favorable reviews, I rarely (or never) continue to use the reviewed product. It seems a bit fraudulent to advertise things to my readers that I don’t use. But books are different. It is a rare book about diabetes that I don’t learn from or at least get inspiration from. Plus I want to support the authors of the Diabetes Online Community (DOC).
I was given the opportunity to read and review Stacey’s second book, Still The World’s Worst Diabetes Mom. In general I turn down most opportunities of free stuff because although I usually write favorable reviews, I rarely (or never) continue to use the reviewed product. It seems a bit fraudulent to advertise things to my readers that I don’t use. But books are different. It is a rare book about diabetes that I don’t learn from or at least get inspiration from. Plus I want to support the authors of the Diabetes Online Community (DOC).

 The title of this blogpost might indicate that I think Covid has gone away and is no longer a risk.
The title of this blogpost might indicate that I think Covid has gone away and is no longer a risk. Covid seriously with masks and vaccines. Even still, three of the four parents have had the virus in the last 6 months as have six of the seven grandchildren.
Covid seriously with masks and vaccines. Even still, three of the four parents have had the virus in the last 6 months as have six of the seven grandchildren. I started Duolingo Spanish in 2020 and am now at Day 752 of daily Spanish lessons. I have learned a lot but am miles away from being a fluent Spanish speaker. I am currently on Unit 50 with Unit 211 as the end goal. I can read many things in Spanish and understand random words from Spanish speakers. I occasionally stumble through a sentence or two with my grandchildren’s nanny from South America.
I started Duolingo Spanish in 2020 and am now at Day 752 of daily Spanish lessons. I have learned a lot but am miles away from being a fluent Spanish speaker. I am currently on Unit 50 with Unit 211 as the end goal. I can read many things in Spanish and understand random words from Spanish speakers. I occasionally stumble through a sentence or two with my grandchildren’s nanny from South America.
 Every ten days my diabetes mental health is in jeopardy.
Every ten days my diabetes mental health is in jeopardy. Or maybe I am lucky and get a number. I take a BG test with my meter. 94
Or maybe I am lucky and get a number. I take a BG test with my meter. 94



 There is a nursery rhyme about going to St. Ives in which there are seven wives, seven sacks, seven cats, etc.
There is a nursery rhyme about going to St. Ives in which there are seven wives, seven sacks, seven cats, etc.